Supervised by: Yuhui Zhou, BA (Hons). Yuhui is a 5th year medical student at the University of Cambridge. She gained a First class degree in her intercalated year studying Pathology. She has an interest in Cancer & Immunology and has been awarded a Wellcome Trust Biomedical Vacation Scholarship to study host responses to infection.
How has the reallocation of cancer resources during the COVID-19 pandemic had an impact on cancer patients’ diagnoses and treatments?
Introduction:
As with any pandemic or major health crisis, COVID-19, a novel coronavirus that targets the respiratory system, has consumed a lot of major health resources. Despite the efforts of many countries around the world to contain the pandemic, resources still proved insufficient to deal with the crisis, prompting an unfortunate necessity of drawing resources from other areas of medicine, one of which has been oncology.
Due to the high number of COVID-19 cases and the mortality rate of said cases, resources have had to be focused on COVID patients. Fewer resources are therefore available for patients suffering from other ailments. While the ethics of the situation has been the topic of many debates, the fact of the matter is that resources have been drawn from cancer patients, leading to more cases of delayed care and lower survival rates. This literature review aims to compare the state of resource allocation before and during the pandemic.
Background on Cancer:
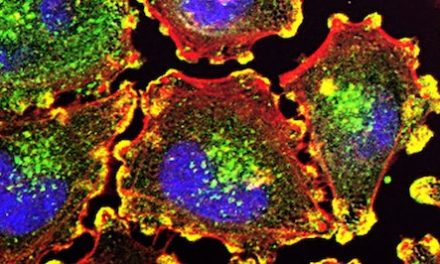
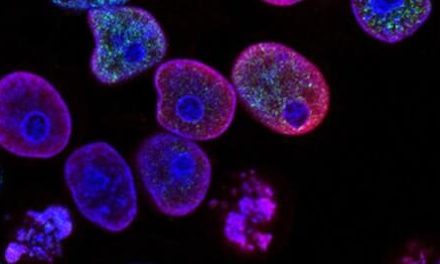
Cancer is a complex disease with many forms, which occurs as a result of rapid and uncontrolled cell reproduction. Cell proliferation in the human body is controlled by proto-oncogenes and tumour suppressor genes. When these proto-oncogenes mutate, they may become carcinogenic and reproduce excessively as malignant cells. Tumours comprised of these cells may then form at nearby and distant sites, disrupting the body’s functions and threatening survival. Cancer develops and becomes more aggressive over time (Weinberg, 1996), with no presently known cure and almost 10 million cancer deaths in 2020 (World Health Organization, 2021), meaning early diagnosis and treatment are incredibly important.
Resources Needed in Cancer Treatment and Diagnosis:
Cancer diagnoses may occur through screening programs, such as the bowel, cervical, and breast cancer screening programs currently provided by the National Health Service (NHS) in the UK, referrals to specialists, and emergency presentation cases (Cancer Research UK, 2021). However, during the COVID-19 pandemic both human and non-human resources, such as accident and emergency doctors, ventilators, and hospital beds (Kutikov et al., 2020) have been redistributed away from this focus. Cancer screening was also halted at the beginning of the pandemic at the recommendation of the American Cancer Society, in an attempt to minimize infection in healthcare settings and prioritize urgent needs (American Cancer Society, 2021). A study published in ‘Frontiers in Oncology’ showed that there was also a significant decline in many diagnosis techniques such as imaging procedures, biopsies, low-dose computed tomography (LDCT), and region-specific tests such as colonoscopies, gastroscopies, sigmoidoscopies and mammographies (Alkatout et al., 2021). Treatment pathways have also differed as a result of COVID-19, with patients being unable to access hospitals for surgeries that are often considered non-emergency or elective (Whittaker et al., 2021) and the delay of radiotherapy treatments being recommended (Hartman et al., 2020). Haemotology and oncology clinical research trials have also been widely suspended, both to reassign staff in order to manage the influx of COVID-19 patients, and to focus on COVID-19 vaccine and testing research (Saini et al., 2020).
Cancer Survival Rates:
Cancer screening, treatment and research were not prioritised during the COVID-19 pandemic, and this has had a clear impact on both the physical and mental wellbeing of patients. A study by Camille Maringe et al. estimated the impact of delays in diagnosis due to COVID-19 on cancer deaths in England with 93,607 English NHS cancer patients, aged 15 to 84. These patients were reallocated diagnostic pathways, from non-urgent and screening referral pathways to urgent ones, and net survival at 1, 3 and 5 years after diagnosis was estimated. A 7.9-9.6% increase in breast cancer deaths was predicted, along with, a 15.3-16.6% increase in colorectal cancer deaths, a 4.8-5.3% increase in lung cancer deaths, and a 5.8-6.0% increase in oesophageal cancer deaths up to 5 years after diagnosis (Maringe et al., 2020). Another investigation found that patient age, cancer type, and cancer stage were important factors in estimating the extent to which delayed treatment would affect integrated survival rates. For example, delayed rather than immediate treatment is estimated to have a minimal impact on prostate cancer patients, whereas the increase in cancer-specific mortality far exceeded the decrease in COVID-19-specific mortality in pancreatic cancer patients (Hartman et al., 2020). It is evident that diagnostic delays due to the COVID-19 pandemic have resulted in large increases in avoidable cancer deaths in England, and policies must be put in place to allocate resources accordingly in the future. However, it is also important to note that these figures are estimates and not collected data, as we are unable to record 5-year survival rates less than 5 years into the pandemic. The case mortality rates in the study by Holly E. Hartman et al. (2020) also relies on multiple assumptions made from available data on worldwide COVID-19 infections, the impact of comorbidities for cancer-specific survival, and clinical chemotherapy treatments.
Ethics of Resource Allocation in a Pandemic:
From late 2019 to date, there have been many more patients requiring resources than there are resources available, so it is important to consider all aspects of medical ethics. Medical ethics is often categorised into four pillars: autonomy – the patient’s right to privacy and a choice in their care; beneficence – the intent of doing good for the patient; non-maleficence – the intent of not doing any harm to the patient; and justice – respecting the law, fair allocation and distribution of limited resources, and treating all patients equally and equitably (Nisselle, 2015). During a pandemic, patient autonomy is significantly decreased as it is important to consider the needs of the entire population, rather than an individual (Al-Benna, 2020). Therefore, operating theatres and surgeons may be allocated to COVID-19 treatment, regardless of the wishes of a cancer patient waiting for non-essential surgery. Sammy Al-Benna highlights the importance of maximising benefits and saving as many lives or years of life as possible in an article regarding resource allocation during the COVID-19 pandemic, by giving priority to the worst off and prioritising healthcare professionals (Al-Benna, 2020). Another article by Ezekiel J. Emanuel et al. (2020) concurs that maximising benefits is the most important value in a pandemic, and suggests that patients should be treated on a first-come, first-served basis in order to maintain a just medical system.
Conclusion:
The COVID-19 pandemic has had a severe effect on the allocation of medical resources, which has put a serious strain on the limited resources available. This literature review aimed to compare the differences between the allocation of resources before and during the COVID-19 pandemic. From the research conducted, it is evident that the field of oncology has been heavily hit, due to the reassigning of resources away from the care and treatment of cancer patients for use in the care of COVID-19 patients. This diversion of resources away from the care of cancer patients has resulted in patients being unable to receive the treatments that they need, including screenings and biopsies. This decrease in the standard of care has resulted in the diagnosis and treatment of many cancer patients becoming severely delayed which has, in turn, resulted in a decrease in the survival rates of cancer patients overall. Unfortunately, the decision as to how the few remaining resources available should be allocated has resulted in an ethical dilemma. It is difficult to determine the most efficient strategy for resource allocation and which aspects of cancer care should be regarded as more important, with more resources distributed to them. Overall, there appears to have been a decrease in the amount of resources allocated towards cancer care as a direct result of the COVID-19 pandemic, which has had and is having a negative impact on the treatment of cancer patients.
Bibliography:
- Weinberg, R. A. (1996). How cancer arises. Scientific American, 275(3), 62-70. https://doi.org/10.1038/scientificamerican0996-62
- Cancer Research UK. (2021, February 5). Cancer screening and diagnosis statistics. https://www.cancerresearchuk.org/health-professional/cancer-screening-and-diagnosis-statistics#heading-One
- Kutikov, A., Weinberg, D. S., Edelman, M. J., Horwitz, E. M., Uzzo, R. G., & Fisher, R. I. (2020). A War on Two Fronts: Cancer Care in the Time of COVID-19. Annals of internal medicine, 172(11), 756–758. https://doi.org/10.7326/M20-1133
- American Cancer Society. (2021, April 23). Cancer screening during the COVID-19 pandemic. Information and Resources about Cancer: Breast, Colon, Lung, Prostate, Skin. https://www.cancer.org/healthy/find-cancer-early/cancer-screening-during-covid-19-pandemic.html
- Hartman, H. E., Sun, Y., Devasia, T. P., Chase, E. C., Jairath, N. K., Dess, R. T., Jackson, W. C., Morris, E., Li, P., Hochstedler, K. A., Abbott, M. R., Kidwell, K. M., Walter, V., Wang, M., Wang, X., Zaorsky, N. G., Schipper, M. J., & Spratt, D. E. (2020). Integrated Survival Estimates for Cancer Treatment Delay Among Adults With Cancer During the COVID-19 Pandemic. JAMA oncology, 6(12), 1881–1889. https://doi.org/10.1001/jamaoncol.2020.5403
- Alkatout, I., Biebl, M., Momenimovahed, Z., Giovannucci, E., Hadavandsiri, F., Salehiniya, H., & Allahqoli, L. (2021). Has COVID-19 Affected Cancer Screening Programs? A Systematic Review. Frontiers in oncology, 11, 675038. https://doi.org/10.3389/fonc.2021.675038
- Whittaker, T. M., Abdelrazek, M., Fitzpatrick, A. J., Froud, J., Kelly, J. R., Williamson, J. S., & Williams, G. L. (2021). Delay to elective colorectal cancer surgery and implications for survival: a systematic review and meta-analysis. Colorectal disease : the official journal of the Association of Coloproctology of Great Britain and Ireland, 23(7), 1699–1711. https://doi.org/10.1111/codi.15625
- Maringe, C., Spicer, J., Morris, M., Purushotham, A., Nolte, E., Sullivan, R., Rachet, B., & Aggarwal, A. (2020). The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. The Lancet. Oncology, 21(8), 1023–1034. https://doi.org/10.1016/S1470-2045(20)30388-0
- World Health Organization. (2021, March 3). Cancer fact sheet. WHO | World Health Organization. https://www.who.int/news-room/fact-sheets/detail/cancer
- Saini, K. S., de Las Heras, B., de Castro, J., Venkitaraman, R., Poelman, M., Srinivasan, G., Saini, M. L., Verma, S., Leone, M., Aftimos, P., & Curigliano, G. (2020). Effect of the COVID-19 pandemic on cancer treatment and research. The Lancet. Haematology, 7(6), e432–e435. https://doi.org/10.1016/S2352-3026(20)30123-X
- Nisselle, P.. (2015, July 1). Essential learning: Law and ethics. Medical Protection. https://www.medicalprotection.org/uk/articles/essential-learning-law-and-ethics
- Sammy Al-Benna. (2020, August 7). Sword of Damocles: Application of the ethical principles of resource allocation to essential cancer surgery patients requiring beds in limited supply during the COVID-19 pandemic. European Surgery. https://link.springer.com/article/10.1007/s10353-020-00655-y#citeas
- Ezekiel J. Emanuel, Govind Persad, Ross Upshur, Beatriz Thome, Michael Parker, Aaron Glickman, Cathy Zhang, Connor Boyle, Maxwell Smith, James P. Phillips. (2020, May 21). Fair allocation of scarce medical resources in the time of COVID-19 | NEJM. New England Journal of Medicine. https://www.nejm.org/doi/10.1056/NEJMsb2005114