Supervised by: Amanda Liu, BEng, MSc. Amanda spent her undergraduate years studying Biochemical Engineering at UCL (University College London), where she was awarded First Class Honours. She then completed her Master’s degree in Clinical and Therapeutic Neuroscience at the University of Oxford. She is currently studying Medicine (Graduate Entry) at the University of Cambridge.
Globally, cardiac illnesses are a leading cause of death. The largest cause of death and illness in the United States is heart attacks, which affect 28 million Americans. Seventy percent of 6 million Americans with heart failure have ischemic cardiomyopathy diagnoses. This occurs when a previous heart attack that damaged the heart muscle has induced chronic heart failure. There are risk variables that cannot be changed and risk factors that may be changed. Age, gender, low birth weight, race or ethnicity, and genetic characteristics are risk factors that cannot be changed. Modifiable risk factors are hypertension, exposure to cigarette smoke, diabetes, atrial fibrillation and certain other cardiac conditions, dyslipidemia, carotid artery stenosis, sickle cell disease, postmenopausal hormone therapy, poor diet, less physical activity, obesity, and body fat distribution. Finally, there are a number of risk factors that may be changed, including metabolic syndrome, drug and alcohol abuse, oral contraceptive use, sleep apnoea, migraines, hyperhomocysteinemia, elevated lipoprotein(a), elevated lipoprotein-associated phospholipase, hypercoagulability, inflammation, and infection.
The heart muscle needs a constant supply of oxygen-rich blood to keep it fuelled and to keep pumping. A blockage in an artery interrupts that blood flow during a heart attack. Without blood, the portion of the heart supplied by the afflicted artery starts to die and develops scar tissue. Heart failure may develop as a result of this damage over time, particularly if heart attacks closely follow one another. 117,000 Americans are waiting for organ transplants, but there aren’t enough available organs to go around. Cardiomyocytes, the cells that produce contractile force in a healthy heart, are damaged by cardiac disorders. This, in turn, has an impact on the heart muscles, and there is a chance that scar tissue will form. Scar tissue can obstruct the heart’s normal function and raise the risk of irregular cardiac rhythms. The heart will eventually become larger and less able to pump effectively as a result of scar tissue overloading the blood flow and stretching the cardiac cells. Those who have had a heart attack, therefore, may need to take medications and undergo other treatments for the rest of their lives in an effort to prevent further heart attacks and improve their heart’s functionality. However, without treatment, this ultimately results in heart failure and, frequently, deaths. Although they are available, medical and surgical procedures are not incredibly effective. Existing treatments lessen the risk of further heart attacks, stop further heart muscle damage, and lower early mortality rates. However, as scar tissue formation following myocardial infarction results in irreversible damage to the heart function, therapy is required to improve the infarcted area by replacing the affected cells. Therefore, using stem cells to regenerate heart tissue may be a better therapeutic strategy.
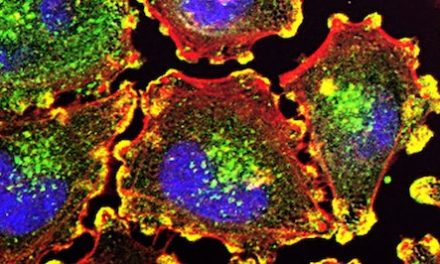
By regenerating lost and defective cardiac muscle cells, stem cell therapy has the ability to replace damaged tissues with healthy tissue, which is something that conventional medications are unable to do. The adult heart’s endogenous capacity for regeneration is still heavily disputed. Adult cardiomyocytes (CMs) are known to regenerate throughout life in response to wear and tear or after injury, but the exact rate and cause of this occurrence are still unknown. When taking into account that adult CMs are terminally differentiated cells, the adult heart contains resident cardiac/stem progenitor cells (CSCs/CPCs), whose discovery and characterization was initially enough to explain CM renewal in response to physiological and pathological stressors. However, certain recent genetic fate map studies that have been shown to have significant shortcomings have called into doubt the significance of CSCs in the development of CMs in the adult heart. Adult and embryonic stem cells both possess the capacity for self-replication and the capacity to differentiate into a variety of specialized cells. The most critical tool in regenerative medicine is therefore evolving to be stem cells. These cells are capable of developing into cardiomyocytes. Studies on mouse embryonic stem cells, which were the first to be identified, supplied the initial information. They were discovered in 1981 by scientists using 100-cell stage mouse embryos. These embryos are made up of blastocysts, hollow balls of cells. A blastocyst, which is hardly wider than one eyelash, contains an inner wall thickening known as the inner cell mass. It would create the complete fetus in a uterus, with all of its membranes, including the amnion. When mouse blastocysts are cultured in a petri dish, the outer layer of cells soon collapses, and undifferentiated cells from the inner cell mass spontaneously form clumps that can be cultured to yield embryonic stem cells. These can grow and divide for long periods in an undifferentiated state. However, when injected back into a mouse blastocyst, they react to physiological stimuli, and mature cells derived from those stem cells develop in nearly every tissue of the embryo. For this reason, embryonic stem cells are termed pluripotent, from the Greek for “many capabilities.”
Surgeries such as organ transplants, surgical reconstructions, and installations of mechanically artificial devices and/or administrations of metabolically derived products are currently more widely used as a means to regain vascular function; however, they are overly invasive, require lengthy hospitalization, and cost incredible amounts. Another option could be prescribed drugs if they were able to reverse the effects of the cardiac disease and not simply slow the progression of heart failure – they are not foolproof treatments and serve only to make patients feel better and decrease the heart’s workload. Therefore, cell therapy comes into play with hopes of using reparative tools to restore, renew, and, most importantly, recycle patients’ proper reparative capacity. To do so, stem cells, with the help of a catheter, are injected into the heart to replace damaged tissue with new tissue, which is stimulated to grow by the said injected cells.
During the process, there are a couple of details that call for attention to be able to provide better results in the long term, like the selection of the cell type for one, or even the number of cells required. As for the appropriate route of administration that kickstarts regeneration, in this case, it happens to be by mode of injection. Contrary to typical vaccine syringes, these injections happen to be more precise catheter-guided transendocardial, intracoronary, transvenous, and transepicardial injections, which translates to injections during which a needle can be inserted into various parts of the heart, depending on where the stem cells are needed most to help regenerate cardiac tissue growth. It should be noted that not all stem cells are injected – it is a trial process. In fact, particular cells used for the therapy, mesenchymal stem cells, are less likely to stimulate an immune response and rejection than most other stem cells. Still, all the selected cells should have control over their migration, proliferation, and differentiation both in vivo and ex vivo in order to fulfil their task of improving vessel density, decreasing fibrosis, and increasing survival rates even in non-ischemic heart failures.
With just one injection into the heart muscle during a cardiac catheterization procedure, stem cells have the ability to repair muscular tissues and reduce inflammation. That’s because, after a trial and error process, researchers have tested different quantities in order to observe which has the most effect on the human heart. In total, three different doses of stem cells in injections were tested: 20 million cells, 100 million cells, and 200 million cells, and ultimately the best dose that was agreed upon was surprisingly the lesser one of 20 million stem cells. Generally, the application of the sentence “the more, the better” is prominent, but in this case, the lowest dose was able to effectively improve the heart pumping ability of the heart as well as diminish the extent of the scar tissue. As a treatment replacing overly-invasive surgical procedures, stem cell therapy combines the medical injection technique known to us presently, as well as the modern, cutting-edge stem cell research to improve the quality of life and overall health of many ailing with this illness across the globe.
The way this approach to treating this cardiac illness was breached was due to thorough research of cardiomyocytes and their replication inside the heart. As the human heart is considered the first organ to have fully developed since it is fairly well defined and tuned, theoretically speaking, the heart potentially has the capacity to regenerate since cardiomyocytes, cells responsible for the actual heartbeat, may be capable of cell division. In addition, a typical adult heart contains a cardiac stem cell niche, which means that a fully-fledged heart could be capable of differentiating into cardiomyocytes and other cardiac-associated cell types. The sole caveat remains that these functions remain deactivated even during serious injury; therefore, there are three options to induce this regeneration of previously damaged heart tissue. One can either proceed by activating endogenous cardiomyocytes to divide, by coaxing an endogenous population of stem cells to divide and differentiate, or by adding exogenous cell-based therapy to replace the damaged cardiac tissue. In other terms, all three possibilities necessitate the injection of stem cells to activate this regeneration function that the heart hypothetically holds.
Results
- Injections: “studies in comparison with routine therapies have shown promising results by significantly improving vessel density, inhibiting apoptosis of myocytes, decreasing fibrosis, and increasing survival rate even in non-ischemic heart failures”
- According to Joshua Hare, M.D. (director of the Interdisciplinary Stem Cell Institute at the University of Miami Miller School of Medicine and the lead author of the study), there are clinically significant improvements even in patients who had heart attacks years before treatment
-
- Both donor AND recipient stem cells substantially reduced the amount of scarring
- Encouraging results: modern-day medicine may improve to the point of truly being able to repair heart attack damage to the heart because, as of now, medicine = mostly therapies to make patients feel better and decrease the heart’s workload
-
and:
- Therapy enhanced heart pumping ability
- Due to heart failure, hearts become more enlarged; however, this treatment caused the heart to return to its previous “regular” size
The results of these studies were very promising in terms of stem cells’ applications in damaged heart muscles. Currently, therapies for heart failure aim to decrease the workload of the heart in order to improve patients’ quality of life. However, stem cell therapies have shown us the possibility of repairing damaged heart tissue and reversing the damage caused by heart attacks. According to the study carried out at Johns Hopkins University, patients with either autologous or allogeneic stem cells injected were monitored for complications, such as heart attacks, strokes, deaths etc. After 12 months, all of the patients were still reported to be alive. The researchers were particularly interested to see if patients’ immune systems would reject allogeneic stem cells. Only 3.7 percent of the patients receiving the donated cells had such a response. Furthermore, patients in both arms of the study experienced a reduction in scar tissue, which increased the heart’s pumping ability and decreased the possibility of experiencing arrhythmias. Additionally, the size of many patients’ hearts became more normal, which is another contributing factor to the heart’s pumping ability. Aside from the improvements in the heart muscles, there were significant changes in patients’ living standards. Many patients were able to walk farther on a six-minute walking test and reported improved quality of life on a questionnaire administered multiple times during the 12-month study period. According to Joshua Hare, M.D. (director of Interdisciplinary Stem Cell Institute at the University of Miami Miller School of Medicine and the lead author of the study), there are clinically significant improvements even in patients who had heart attacks years before treatment. Both donor and recipient stem cells reduced the amount of scarring substantially. He states that modern-day medicine can improve to the point of truly repairing heart attack damage.
Further studies, compared with the routine therapies, have shown promising results by significantly improving vessel density, inhibiting apoptosis of myocytes, decreasing fibrosis, and increasing survival rate even in non-ischemic heart failures.
Given the complexity of cardiovascular problems, which include a variety of disease patterns and pathologic causes, it may be challenging to offer a single therapeutic approach to all patient subgroups. Future plans should therefore focus on more individualized therapy where the choice of the best cell type, dosage, and delivery method is influenced by the specifics of the patient’s ailment. The limited vitality of implanted stem cells for heart repair is a significant barrier in this field. The solutions examined are intended to improve and create appropriate methods for treating cardiac diseases. Any organization’s attempts that use a particular cell type are said to produce more effective outcomes than others. This has led to disagreements over the cell types that can produce beneficial results, which has consequently led to a lack of understanding among doctors. Even though cell treatment is currently in the spotlight, involvement in it has therefore declined. Future application problems, therefore, depends on a clear validation of cell therapy with regard to source, administration strategy, dosage, and intended result. It is essential to replicate these outcomes in order to advance the technology.
The employment of alternative tactics is frequently hampered by ethical issues, which must be clearly defined in light of the advantages the medical industry would gain. Although embryonic stem cells show potential for cardiac cellular treatment, their usage in clinical settings presents moral and legal issues. An infarcted heart can benefit from both adult and ESC treatment. There is still debate over the optimum cell type to use as a source for transplantation into an ischemic heart because there are no established cell markers. The optimal stem cell types and their sources for clinical use need to be studied. ESCs show potential for myocardial cellular treatment, but their medical applications are fraught with moral dilemmas and public controversy. NIH claims that the production of stem cells requires the eradication of human embryos. Research on embryonic stem cells raises two opposing viewpoints: one is that using stem cells might be able to reduce suffering, while the other is that human life should be respected. Is it worthwhile sparing someone pain when the cost is destroying human life? By reprogramming somatic cells to create induced pluripotent stem cells, the ethical problems unique to ESC research can be overcome. Human ESCs produce cardiomyocytes in vitro, but it is yet unknown if undifferentiated human ESCs are capable of regeneration following in vivo engraftment.
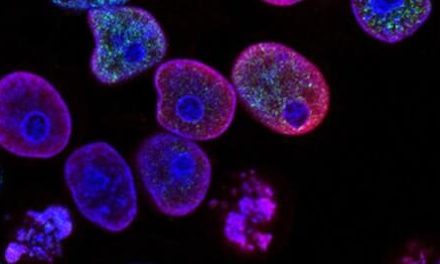
An artificial womb was utilized to produce synthetic mouse embryos for eight days by stem cell researchers in Israel. This breakthrough provides a glimpse into a fascinating, perhaps contentious area of science that one day may be used to create human replacement organs. Scientists developed synthetic embryos from a collection of embryonic stem cells that closely resembled real mouse embryos, complete with folded brain tissue, a beating heart, and blood circulation. The mouse embryos developed in an artificial womb for eight days, or around one-third of a mouse pregnancy, until they ceased growing. But as the models become more like the real thing, they also venture into morally ambiguous areas. When do artificial embryos resemble genuine ones enough to merit protections comparable to those given to actual embryos? The study is nowhere near being able to grow a mouse outside of the womb, much less a human. While the researchers were successful in creating a full synthetic embryo from embryonic stem cells as a proof of concept, it was a very error-prone process, and only a small percentage of the embryos went on to develop the first stages of a beating heart and other organs. Instead of replacing reproduction, the technology is intended to be utilized to develop synthetic human embryo models that could yield organ precursors that could be researched and potentially employed therapeutically.
The main obstacle to the therapeutic use of ESCs is the development of teratomas by undifferentiated cells since these cells might not be directed to grow new myocardium after transplantation. Before considering ESC-based therapy, the malignant tumorigenic potential of ESCs must be identified, and the possibility of teratoma formation must be completely eliminated. Through guided cardiopoiesis, heart tissue is produced without teratomas thanks to the definitive engagement of stem cells. Cardiopoietic programming provides a method for regeneration that is resistant to tumors. Embryonic stem cells must first be processed in vitro and differentiated along tissue-specific lineages to produce, for example, adult stem cells or differentiated progeny before being transplanted into human patients. However, when a full patient agreement is secured, adult stem cells do not pose the same ethical problems. Adult stem cells, however, are highly uncommon in vivo, have relatively low multipotency, and are often challenging to expand ex vivo. Additionally, adult stem cell collection from patients is intrusive and comes with a lot of danger and discomfort for the patient. An unrelated donor’s stem cells run the risk of being rejected by the body’s immune system. Additionally, hazardous cardiac rhythms could result from the implanted cells if they are unable to connect with the heart’s intricate electrical system (arrhythmias). However, side effects haven’t been a significant problem thus far, which has motivated researchers to continue. To determine the role stem cell therapy will play in treating heart disease, more extensive long-term studies are required.
The therapy strategy is already being commercialized, which is another worrying aspect. Premature trials may give patients false optimism and siphon funds away from the fundamental research required to develop more effective therapies. Companies that provide therapies for conditions ranging from Parkinson’s disease to heart failure have sprung up as a result of the stem cell method, which has led to the international commercialization of various kinds of therapy. But there is still no proof of these medicines’ efficacy. Additionally, it is an extremely costly procedure that restricts and separates access. As a result, this method is not a very universal one.
Conclusion
After the injection trial, patients were able to walk farther on their 6-minute walking test & reported improved quality of life. There are 6 main breakthroughs of stem cell therapy: safety establishment in intracoronary delivery, the possibility of therapeutic regeneration, allogeneic cell therapy, increasing mechanistic insights, sparkling clinical efficacy, and progress to phase 2/3 studies. Although there is more to investigate and learn about the mechanism of action for all these stem cell-based therapies, it remains a promising field of research.
References
- https://www.hopkinsmedicine.org/news/media/releases/stem_cell_therapy_safely_repairs_damaged_heart_muscle_in_chronic_heart_failure_patients_study_shows
- https://www.mayo.edu/research/centers-programs/center-regenerative-medicine/focus-areas/cardiac-regeneration
- https://pubmed.ncbi.nlm.nih.gov/32466282/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4591785/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3103911/
- https://www.sciencedirect.com/science/article/abs/pii/S0143400411002189 – where are the stem cells coming from
- https://www.jstor.org/stable/26058169 – embryonic stem cells for medicine
- https://www.sciencedirect.com/science/article/abs/pii/S135727250300356X
- https://link.springer.com/protocol/10.1007/978-1-4939-3584-0_4
- https://go.gale.com/ps/i.do?id=GALE%7CA367420948&sid=googleScholar&v=2.1&it=r&linkaccess=abs&issn=00280836&p=HRCA&sw=w&userGroupName=anon%7E8bd03668
- Repairing-the-heart-with-stem-cells
- 30121644
- 30396088
- 34630860
- synthetic-mouse-embryo