Supervised by: Yuhui Zhou, BA (Hons). Yuhui is a 5th year medical student at the University of Cambridge. She gained a First class degree in her intercalated year studying Pathology. She has an interest in Cancer & Immunology and has been awarded a Wellcome Trust Biomedical Vacation Scholarship to study host responses to infection.
Thesis statement:
Undoubtedly, COVID-19 has imposed various limitations on patients who are diagnosed with cancer. Coronavirus disease is a highly infectious disease as a result of acute respiratory syndrome (SARS-CoV-2). In order to alleviate the burden on healthcare systems caused by an influx of COVID-19 patients, suspensions of elective surgeries were implemented. This may have led to a decline in cancer diagnoses. Due to the pandemic and the fearful exposure of this virus to patients, healthcare appointments were reduced and replaced with video as well as telephone calls. An example of the impacts this had would be the American Cancer Society. It was estimated that 22 million cancer screenings were missed or cancelled, seen in a precipitous decline in screening rates for colon, cervical and breast cancer – just to name a few. Due to the reasons above, diseases such as cancer would be identified at a later point in time, further resulting in a poor prognosis.
Final question:
To what extent has the COVID-19 pandemic affected cancer screening, diagnosis and treatment and how does this compare to the current situation, pre and post pandemic?
Initial questions:
How has COVID affected national screenings for cancer? How have cancer screenings changed and progressed since COVID-19 limitations were set in place? To what extent have delayed screenings affected cancer diagnoses and treatment?
Introduction
In late December of 2019, the government in Wuhan, China released information concerning dozens of cases of pneumonia with unknown causes. In the days that followed, researchers in China identified a new virus, now known as SARS-CoV-2, or more commonly as the coronavirus. Little was known about the virus, including if the virus was spread via human contact.
By March 2020, numerous cases had been reported throughout the world, and COVID-19 was declared a pandemic. Immediately following the declaration, drastic government-led actions including national lockdown and shelter-in-place orders became prevalent throughout the world, effectively discontinuing normal life practices, including medical appointments and screenings. SARS-CoV-2 is a respiratory virus in nature, leading to symptoms such as fever, cough, fatigue, headache, sore throat, and nausea, and has now been determined to spread through saliva or discharge from the nose. COVID-19 can be diagnosed through polymerase chain reaction testing, or PCR testing, which denotes the presence of the RNA of the virus with a 71% detection rate. According to the World Health Organization, most people infected with COVID-19 will primarily experience mild to moderate respiratory symptoms; however, elderly people and those with comorbidities and immunocompromisation such as heart disease, diabetes, cancer, and chronic respiratory disease are much more susceptible to
chronic illness. In response to the virus, numerous health care facilities and hospitals had to cancel appointments and cancer screenings, using tele-health appointments instead in order to create space for COVID-19 infected patients, leading to a dramatic decrease in cancer screenings throughout the world. In the United States, cancer is the second-highest leading killer. According to the National Cancer Institute, cancer develops through the uncontrollable growth of cells, so early detection is vital in the treatment of various types of cancer in order to slow the growth of rogue cells throughout the body. The purpose of this literature review is to explore the effect of the COVID-19 pandemic on cancer screenings and thus missed diagnoses, while also explaining the future of cancer screenings as compared to pre-pandemic normalities.
Statistics
With regards to breast cancer, 2.3 million women were diagnosed with breast cancer in the year of 2020. The following statistics demonstrate the age-standardised rate per 100,000:
- Belgium – 113.2
- Luxembourg – 109.3
- Netherlands – 105.9
- France (metropolitan) – 99.1
- New Caledonia (France) – 98.1
- Lebanon – 97.6
- Australia – 94.5
- United Kingdom – 93.6
- Italy – 92.8
Many amongst others.
With regards to cervical cancer, 570,000 women were diagnosed with cervical cancer in the year of 2018. The following statistics demonstrate the age-standardised rate per 100,000:
- Swaziland – 75.3
- Malawi – 72.9
- Zambia – 66.4
- Zimbabwe – 62.3
- Tanzania – 59.1
- Burundi – 57.4
- Uganda – 54.8
- Lesotho – 52.1
- Madagascar – 51.6
- Comoros – 50.9
Cervical cancer is typically associated with HPV (Human Papillomavirus).
With regards to leukemia (also acknowledged as blood cancer), 60,530 people are expected to be diagnosed with leukemia in the year of 2020.
Below, are the various types of leukemia:
➔ Acute lymphocytic leukemia.
➔ Acute myelogenous leukemia.
➔ Chronic lymphocytic leukemia.
➔ Chronic myelogenous leukemia.
Leukemia is classified in two parts: Acute leukemia as well as chronic leukemia. Lymphocytic leukemia affects the lymphoid cells or lymphatic tissue, whereas myelogenous leukemia, affects the myeloid cells in the body.
With regards to colorectal cancer, over 1.8 million people were diagnosed with colorectal cancer in the year of 2018. This type of cancer more typically occurs in men than in women. The following statistics demonstrate the age-standardised rate per 100,000:
- Hungary – 51.2
- South Korea – 44.5
- Slovakia – 43.8
- Norway – 42.9
- Slovenia – 41.1
- Denmark – 41.0
- Portugal – 40.0
The impact of cancer screening during the COVID-19 pandemic to health
COVID-19, which began in December of 2019, has become a pandemic on a global scale. Lockdown schemes have been implemented throughout countries around the world. As a result, cancer screening check ups were halted in order to prioritize the resources for COVID-19 screening, treatment and research, and reduce the risk of the spread of COVID-19 in healthcare settings, suggested by American Cancer Society (Cancer Screening During the COVID-19 Pandemic, n.d.). According to a systematic review by Alkatout et al. (2021), it was reported that many individuals avoid contracting specialists due to fear of being infected by COVID-19. Moreover, the patients and hospital staff are experiencing fear and anxiety. Their findings also address the decline of cancer screening procedures including biopsies, colonoscopies, gastroscopie, sigmoidoscopie, stool tests, low-dose computed tomography (LDCT), mammography, Pap tests, human papillomavirus (HPV) testing, colposcopies, laparoscopies, and melanoma screening.
Carolyn Muller, MD, a chief of gynecologic oncology at the University of New Mexico, asserted that, “A delay in screening can cause a delay in diagnosis and in turn cause poor outcomes”. She further stated that this is because the cancer is more likely to progress to a more advanced state (Scherer, 2021). In Alkatout et al.’s work, their discussion concluded that there will be more life loss because of the cancer screening delay in Canada; additionally the postponement of cancer diagnosis and treatment will have a tremendous impact on survival rate and life-years are mitigated.
The importance of regular cancer screening:
Within various health systems, physicians are obligated to encourage early cancer detection and regular cancer screenings, despite the challenges presented by lead time and length bias. Undoubtedly, regular cancer screening provides the opportunity to detect cancer at its early stages, allowing for prompt treatment in order to slow the growth of malignant cells. In most cases, doctors encourage routine screening for breast, colon, cervix, and prostate cancer; however, if a patient is genetically predisposed to another form of cancer that is not regularly screened for amongst the general population, they may be given the option of voluntary screenings as well. Despite the perceived benefits of early detection, it is also important to acknowledge lead time and length bias.
Lead-time bias refers to diagnosing the cancer earlier than it would otherwise have been but, despite earlier detection, the course of the disease does not change. Here is an example below of a 67 year old, male patient with persistent coughing leading to a lung cancer diagnosis, presented by Wegwarth et al. in the Annals of Internal Medicine.
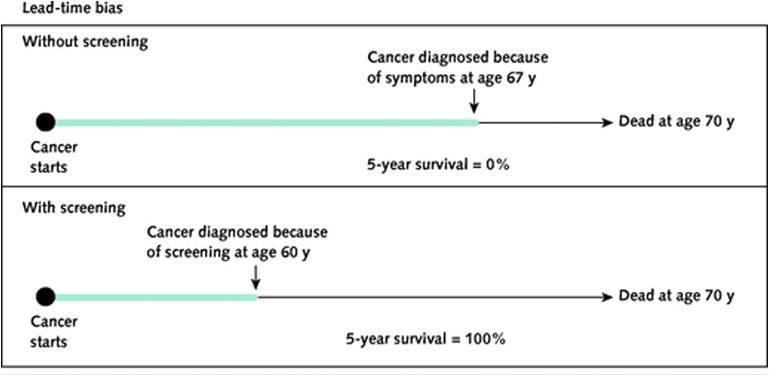
Despite an earlier diagnosis via screening seven years earlier, the patient’s disease still retained the same course, but the 5-year survival rate dramatically increased to 100% with a screening-based diagnosis. Regardless, the patient lives for the exact same amount of time, even with an early diagnosis.
Length bias is another factor in determining the importance of routine cancer screenings, referring to the fact that screening-based cancers (such as breast, prostate, colon, and cervix) are often less aggressive and slower-growing. Because these cancers develop more gradually, they can exist malignantly in the body longer than symptoms for fast-growing cancers develop. Length bias can possibly lead to overdiagnosis, in which cancers that do not require treatment are diagnosed. According to the National Cancer Institute, “19% of screen-detected breast cancers and 20% to 50% of screen-detected prostate cancers are overdiagnosed.”
Nevertheless, according to Dr. Lyndsay Willmott, a gynecologic oncologist at Arizona Oncology, routine screening presents an “important chance to discuss and evaluate your risks and make any adjustments that can help minimize your chances of developing cancer.” During the COVID-19 pandemic alone, it is estimated that colon cancer screening in the US dropped 86% and screening for breast and cervical cancer dropped 94%. Even with a gradual return to normalcy, the numbers expected for routine cancer screenings have not returned to pre-pandemic standards.
Screenings
A patient could undergo one of the following screenings in order to detect colorectal cancer:
- Colonoscopy – a tube is inserted into the rectum as well as the colon. This enables the doctor or practitioner to have a look for any potential cancer or polyps.
- Computed tomography – used as an alternative for a typical colonoscopy.
- Sigmoidoscopy – a tube is inserted into the rectum as well as the lower colon in order to recognise any cancer, polyps or other potential abnormalities.
- Fecal occult blood test (FOBT) + fecal immunochemical test (FIT) – These tests are used to detect blood in the stool, which could possibly be a sign of cancer.
- Double contrast barium enema (DCBE) – this is dedicated to patients who aren’t able to undergo a colonoscopy. Therefore, they are given an enema containing barium. This helps the colon as well as rectum to show clearly on the x-rays.
- Stool DNA tests – analyses the DNA from the stool sample of a patient.
As for breast cancer, a patient could undergo one of the following screenings:
- Mammogram – best method to detect cancer at an early stage. Women should regularly have mammograms done as it lowers the risk of death from breast cancer.
- Breast Magnetic Resonance Imaging (MRI) – An MRI as well as a mammogram is done for women who are at a high risk of developing cancer.
The following screenings may be offered to a patient at risk of cervical cancer:
- Pap test or pap smear.
- HPV test.
A patient could undergo one of the following screenings to detect risk of leukemia:
- Bone Marrow Aspiration and Biopsy – a sample extracted from the hip bone or any other large bone that could potentially have cancer.
- Chest X-ray or Chest CAT scan – reveals any swollen lymph nodes or potential infections in the chest.
- Spinal tap – the doctor will extract/remove some of the cerebrospinal fluid from the lower part/fraction of your spine. Afterwards, the laboratory will check the fluid extracted from the patient’s body, and examine it in order to detect any leukemia cells.
Understanding the Future of Cancer Screening
In terms of just breast cancer alone, it is estimated that the COVID-19 pandemic led to about 36,000 delayed diagnoses. Furthermore, it is believed that 2,500 cases of cervical cancer received delayed diagnoses along with 18,800 cases of colorectal cancer. Even with the recession of the COVID-19 pandemic and a gradual return to normal healthcare standards, the fear of contracting the virus still discourages people from scheduling cancer screenings. Although cancer screening appointments have begun to return to normal (especially in regards to mammography), they still fall beneath pre-pandemic standards, especially in colonoscopy screenings. This begs the question, what is the future of cancer screenings in a post-pandemic world?
For example, in 2016 the US Preventative Task Force (USPSTF) added an mt-sDNA Cologuard test as a home screening option. Prior to lockdown orders, mt-sDNA testing was far less common than standard colonoscopy screening procedures. While in-office visits were limited during the pandemic, mt-sDNA testing procedures could be performed from home. In the aftermath of the pandemic, mt-sDNA testing continues to grow more popular at a gradual pace.
Conclusion
To conclude this literature review, both men and women need to consider getting screened for cancer on a regular basis, in order to detect any potential cancer cells. However, during the pandemic, cancer screening has become more difficult because resources need to be allocated towards COVID-19 treatments and the reduction of cancer screenings has been considered to prevent the spread of COVID-19 in healthcare settings.
Regular cancer screening and swift treatment for cancer should be protected, as it’s very important; any delays, even just a few months, could allow cancer to progress into more severe states, which, in return, could significantly lower life expectancy. Even after the pandemic’s peak, the data suggested that the worry of contracting COVID-19 is still in place. Therefore, people have missed or cancelled their screening appointments.
We also mentioned various cancer screening options that will be available after the COVID-19 restrictions are lifted, including colorectal cancer, breast cancer and cervical cancer, in addition to leukemia.
Bibliography
Cancer Trends: How Has the COVID-19 Pandemic Affected Cancer Screening? | Everyday Health. (1996-2021) [Online] Available at: https://www.everydayhealth.com/cancer/cancer-trends-how-has-the-covid-19-pandemic-a ffected-cancer-screening/ [Accessed: 11th July 2021]
Cancer (1999-2021) The future of cancer screening after COVID-19 may be at home. [Online] Available at: https://acsjournals.onlinelibrary.wiley.com/doi/10.1002/cncr.33274 [Accessed: 11th July 2021]
ScienceDirect (2021) Effect of the COVID-19 Pandemic on Surgical Breast Cancer Care in the Netherlands: A Multicenter Retrospective Cohort Study [Online] Available at: https://www.sciencedirect.com/science/article/pii/S152682092030207X [Accessed: 11th July 2021]
World Health Organization (2021). Breast cancer. [Online] Available at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer [Accessed: 17th July 2021]
Breast cancer statistics | World Cancer Research Fund International. (n.a) [Online] Available at: https://www.wcrf.org/dietandcancer/breast-cancer-statistics/ [Accessed: 17th July 2021]
Cervical cancer statistics | World Cancer Research Fund International. (n.a) [Online] Available at: https://www.wcrf.org/dietandcancer/cervical-cancer-statistics/ [Accessed: 17th July 2021]
WCRF International. 2021. Colorectal cancer statistics | World Cancer Research Fund International. [Online] Available at: https://www.wcrf.org/dietandcancer/colorectal-cancer-statistics/ [Accessed 17 July 2021].
Alsharif, W., & Qurashi, A. (2021). Effectiveness of COVID-19 diagnosis and management tools: A review. Radiography (London, England : 1995), 27(2), 682–687. https://doi.org/10.1016/j.radi.2020.09.010
Coronavirus. (2021). Coronavirus. [Online]Available at: https://www.who.int/health-topics/coronavirus#tab=tab_1 [Accessed: 17th July 2021]
PubMed. (2021.) Effectiveness of COVID-19 diagnosis and management tools: A review – PubMed. [Online] Available at: https://pubmed.ncbi.nlm.nih.gov/33008761/ [Accessed: 20th July 2021]
Cancer.Net. (2021). Colorectal Cancer: Screening | Cancer.Net. [Online] Available at: https://www.cancer.net/cancer-types/colorectal-cancer/screening [Accessed: 20th July 2021]
Cancer Screening During the COVID-19 Pandemic | Cancer Tests and Coronavirus. (2021). Cancer Screening During the COVID-19 Pandemic | Cancer Tests and Coronavirus. [Online] Available at: https://www.cancer.org/healthy/find-cancer-early/cancer-screening-during-covid-1 9-pandemic.html [Accessed: 20th July 2021]
EverydayHealth.com. (2021). Cancer Trends: How Has the COVID-19 Pandemic Affected Cancer Screening? | Everyday Health. [Online] Available at: https://www.everydayhealth.com/cancer/cancer-trends-how-has-the-covid-19-pand emic-affected-cancer-screening/ [Accessed: 17th July 2021]
Alkatout, Ibrahim et al. “Has COVID-19 Affected Cancer Screening Programs? A Systematic Review.” Frontiers in oncology vol. 11 675038. 17 May. 2021, doi:10.3389/fonc.2021.675038
www.ncbi.nlm.nih.gov. (2021). Has COVID-19 Affected Cancer Screening Programs? A Systematic Review. [Online] Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8165307/ [Accessed: 17th May 2021]
CDC. (2020). What is Breast Cancer Screening? [Online] Available at: https://www.cdc.gov/cancer/breast/basic_info/screening.htm [Accessed: 20th July 2021]
CDC. (2021). What Should I Know About Cervical Cancer Screenings? | CDC. [Online] Available at: https://www.cdc.gov/cancer/cervical/basic_info/screening.htm [Accessed: 20th July 2021]
Leukemia Diagnosis and Screening – The Johns Hopkins Kimmel Cancer Center. (n.a) [Online] Available at: https://www.hopkinsmedicine.org/kimmel_cancer_center/cancers_we_treat/leukemia_pro gram/diagnosis_and_screening.html [Accessed: 20th July 2021]
PubMed. (2021). The Importance of Cancer Screening – PubMed. [Online] Available at: https://pubmed.ncbi.nlm.nih.gov/33099452/ [Accessed 20 July 2021]
Leukemia – Symptoms and causes – Mayo Clinic. [Online] Available at: https://www.mayoclinic.org/diseases-conditions/leukemia/symptoms-causes/syc-2037437 3 [Accessed: 20th July 2021]
The Importance of Preventive Cancer Screening | Blog. 2021. The Importance of Preventive Cancer Screening | Blog. [ONLINE] Available at: https://blog.arizonaoncology.com/the-importance-of-preventive-cancer-screening/. [Accessed: 22nd July 2021]
Cancer.gov. 2021. What Cancer Screening Statistics Really Tell Us – National Cancer Institute. [Online] Available at: https://www.cancer.gov/about-cancer/screening/research/what-screening-statistics-mean. [Accessed: 22nd July 2021]
Harvard Referencing generator: https://www.harvardreferencinggenerator.com/